Every year on November 14th, people worldwide collectively focus on a crucial health issue—diabetes. This day is designated as World Diabetes Day by the United Nations and the International Diabetes Federation, aiming to raise global awareness and consciousness about diabetes. This year marks the 17th World Diabetes Day, with the theme "Everyone Deserves Diabetes Health Management" and the slogan "Know the Risk, Know the Response." This article delves into the background of diabetes, high-risk populations, preventive measures, and more, providing readers with a comprehensive understanding.

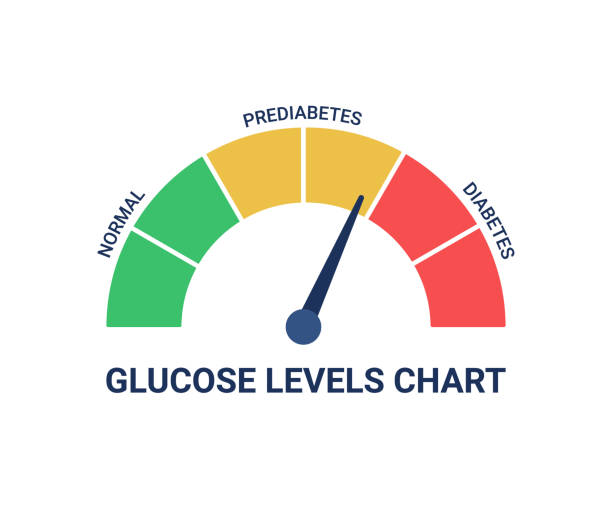
I. What is Pre-diabetes?
Pre-diabetes refers to a condition where an individual's blood sugar levels are higher than normal but have not reached the diagnostic criteria for diabetes. It represents an early stage in the development of diabetes, where the body's response to insulin begins to weaken, and blood sugar control is not as effective as in a normal state.
The primary conditions associated with pre-diabetes include:
◆ Impaired Fasting Glucose (IFG): Fasting blood sugar levels are elevated but do not meet the criteria for diabetes. Typically, this refers to fasting blood sugar levels between 100 mg/dL (5.6 mmol/L) and 125 mg/dL (6.9 mmol/L).
◆ Impaired Glucose Tolerance (IGT): Two-hour blood sugar levels during an oral glucose tolerance test (OGTT) are higher than normal but do not reach the diabetes standard. Usually, this refers to two-hour blood sugar levels between 140 mg/dL (7.8 mmol/L) and 199 mg/dL (11.0 mmol/L).
The presence of pre-diabetes indicates a higher risk of developing diabetes but also offers an opportunity for prevention. Through a healthy lifestyle, balanced diet, moderate exercise, and maintaining a healthy weight, individuals with pre-diabetes may delay or prevent the progression to diabetes. Therefore, proactive lifestyle interventions and regular monitoring are crucial for individuals diagnosed with pre-diabetes. Taking measures promptly may help slow down or prevent the development of diabetes.

II. Who are the High-risk Populations for Diabetes (Adults >18 years old)?
In adults, populations at high risk for diabetes include individuals with one or more of the following risk factors. These factors may increase the risk of developing diabetes. The main risk factors for high-risk populations for diabetes are:
1. Age ≥40 years: The risk of diabetes increases gradually with age.
2. History of pre-diabetes (IGT, IFG, or both): Previously diagnosed with pre-diabetes, i.e., impaired fasting blood sugar or impaired glucose tolerance.
3. Overweight (BMI ≥24 kg/m²) or obesity (BMI ≥28 kg/m²) and/or central obesity: Overweight and obesity are significant risk factors for diabetes, especially central obesity, characterized by abdominal fat accumulation.
4. Sedentary lifestyle: Lack of physical activity and prolonged sedentary behavior increase the risk of diabetes.
5. Family history of type 2 diabetes among first-degree relatives: Direct family members (parents, siblings) with a history of type 2 diabetes.
6. History of gestational diabetes in women: Previously diagnosed with gestational diabetes during pregnancy.
7. High blood pressure: Systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg or undergoing antihypertensive treatment.
8. Abnormal blood lipids: High-density lipoprotein cholesterol (HDL-C) ≤0.91 mmol/L and/or triglycerides (TG) ≥2.22 mmol/L or undergoing lipid-lowering therapy.
9. Atherosclerotic cardiovascular disease (ASCVD) patients: Individuals already suffering from atherosclerotic cardiovascular diseases.
10. History of transient steroid diabetes: Previously experienced transient episodes of high blood sugar.
11. Polycystic ovary syndrome (PCOS) patients or clinical conditions associated with insulin resistance: Such as hirsutism.
12. Long-term use of antipsychotic and/or antidepressant medications and statins: Specific medications may be associated with the development of diabetes.
The presence of these risk factors may make individuals more susceptible to diabetes. Therefore, more frequent diabetes screening and health management become crucial for high-risk populations.

High blood pressure

Sedentary lifestyle

Overweight (BMI ≥24 kg/m²)
III. What are the Symptoms of Diabetes?
The symptoms of diabetes may vary depending on the type and duration of diabetes. However, in general, here are some common symptoms that diabetes may present:
Polyuria (frequent urination): Diabetes patients often feel thirsty because high blood sugar increases the body's water content, leading to frequent urination.
1. Polydipsia (excessive thirst): Due to frequent urination, patients may experience abnormal thirst as a physiological response to fluid loss.
2. Weight loss: Despite increased appetite, the inability of cells to utilize glucose effectively leads to the breakdown of muscle and fat for energy, resulting in weight loss.
3. Fatigue: Diabetes patients may feel tired or weak, possibly due to the body's inability to utilize blood sugar as an energy source.
4. Blurred vision: Elevated blood sugar levels may cause fluid loss from the eyes, resulting in blurred vision. This is usually temporary, and symptoms may diminish with controlled blood sugar levels.
5. Slow wound healing: Diabetes affects the body's ability to heal wounds and injuries, potentially leading to prolonged wound healing.
6. Frequent infections: Diabetes patients are more susceptible to infections, especially in the skin, urinary tract, and respiratory system.
7. Numbness or tingling in extremities (diabetic neuropathy): Long-term high blood sugar can damage the nervous system, causing numbness, tingling, or pain in the limbs.
8. Leg ulcers: Poorly controlled diabetes over an extended period may lead to damage to blood vessels and the nervous system, increasing the risk of lower limb ulcers.
9. Sexual dysfunction: Diabetes may lead to sexual function problems, affecting libido and performance.
These symptoms may not be experienced by every diabetes patient and can sometimes be mild. Especially in the early stages of diabetes, symptoms may be relatively subtle. Therefore, early diabetes screening is crucial for high-risk individuals and those experiencing symptoms. If there are diabetes-related symptoms or risk factors, timely medical examination and diagnosis are recommended.

Fatigue

Polydipsia

Numbness or tingling in extremities
IV. What are the Symptoms of Diabetes Complications?
Diabetes complications arise from the long-term damage caused by high blood sugar to various organs and systems in the body. These complications may develop in diabetes patients, particularly when diabetes is not adequately controlled or treated promptly. Here are some common diabetes complications and their possible symptoms:
1. Cardiovascular disease: Elevated blood sugar may cause vascular damage, increasing the risk of heart disease and stroke. Symptoms may include chest pain, palpitations, shortness of breath, fatigue, etc.
2. Peripheral neuropathy: Prolonged high blood sugar may lead to damage to the nervous system, causing numbness, tingling, pain, or abnormal sensations in the extremities.
3. Diabetic kidney disease: High blood sugar can damage the kidneys, eventually leading to chronic kidney disease. Symptoms may include changes in urine (increased or decreased), swelling, high blood pressure.
4. Diabetic retinopathy: Diabetic retinopathy is one of the most common eye complications in diabetes patients, leading to blurred vision, visual field loss, or blindness.
5. Foot problems: Long-term high blood sugar may lead to damage to foot nerves and blood vessels, increasing the risk of foot ulcers and infections.
6. Hypertension: Diabetes and high blood pressure are often interlinked and mutually affect each other. Hypertension may be an independent risk factor for diabetes complications.
7. High cholesterol: High blood sugar may lead to lipid abnormalities, increasing the risk of atherosclerosis and cardiovascular diseases.
8. Diabetic neuropathy: In addition to peripheral neuropathy, it may also lead to damage to the autonomic nervous system, causing gastrointestinal problems, sexual dysfunction, etc.
9. Diabetic foot: Long-term high blood sugar may lead to reduced sensation in the feet, making them prone to injury, eventually developing into ulcers and infections.
10. Increased risk of fractures: Studies suggest that the risk of fractures may increase in diabetes patients, especially in the elderly.
It is essential to note that the onset of these complications may be gradual, sometimes existing in patients before they are aware of them. Therefore, for diabetes patients, regular health check-ups and blood sugar level control are key to preventing complications. Early detection and appropriate treatment measures can effectively slow down the progression of complications.

V. How to Address the Above Situations?
If your blood sugar is normal and you are at high risk of diabetes, it is essential to maintain a healthy lifestyle, engage in moderate exercise, and regularly monitor metabolic indicators such as blood pressure, blood sugar, blood lipids, and weight.
If you are in the early stages of diabetes, reinforcing your lifestyle is crucial. This includes limiting salt and alcohol intake, adopting a balanced diet, controlling calorie intake, and engaging in high-intensity physical activity for more than 150 minutes per week. If the expected intervention goals are not achieved after six months, drug intervention, such as metformin or acarbose, may be considered.
If you are diagnosed with diabetes, there is no need to worry. According to current medical technology, diabetes is not as daunting as it seems. With timely intervention, diabetes can be effectively reversed, achieving clinical remission and freeing you from glucose-lowering medications. Which groups of people are likely to achieve diabetes reversal?
1. Early diabetes patients: Active lifestyle interventions for early diabetes patients, including a balanced diet, weight control, and increased physical exercise, may help reverse diabetes to some extent.
2. Newly diagnosed diabetes patients: Timely intervention, including lifestyle and dietary improvements, for newly diagnosed diabetes patients may contribute to reversing the progression of diabetes.
3. Overweight or obese diabetes patients: Weight is closely related to diabetes. Through weight control, low-fat diets, and increased exercise, overweight or obese diabetes patients may achieve reversal.
4. Patients with a positive response to lifestyle changes: Some patients are more likely to change their lifestyle, including dietary and exercise habits. For these patients, adherence to a healthy lifestyle may significantly increase the likelihood of diabetes reversal.
5. Young diabetes patients: Younger diabetes patients usually have better metabolic adaptability. By changing their lifestyle, they may find it easier to achieve diabetes reversal.

It's important to note that diabetes reversal is not applicable to everyone, and results may vary from person to person. Individual differences in body condition, diabetes severity, and lifestyle will affect the possibility of reversal. Therefore, any plan to reverse diabetes should be undertaken under the guidance of a doctor and tailored to individual circumstances. Doctors can assess the overall health of patients, provide appropriate advice, and develop personalized treatment plans.